Making prevention an integral part of healthcare
Jan. 2017Prevention in healthcare
Prevention in healthcare. In its Health2020 strategy, the Swiss Federal Council made the development and implementation of a strategy non-communicable diseases a priority in its healthcare policy. Strategic objectives and associated measures were drawn up, together with the addiction strategy and the mental health programme, and approved in late 2016 by the Federal Council and the National Health Policy Dialogue. Prevention and control of non-communicable diseases can be further improved thanks to these measures. One of the main issues underlying the NCD strategy is to improve integration of prevention into healthcare, in order to curb the increasing incidence of chronic diseases as well as further cost increases. But how can this be done? What has been done so far to improve it? And is it possible to estimate the future benefits?
We would all like to lead a healthy and pain-free life for as long as possible. We can make the most important contribution ourselves – by improving our lifestyle. About 70 % of people in Switzerland already pay attention to their diet and 72.5 % get enough exercise. They support their health as much as people who stop smoking and don't drink to excess. This is because many of the non-communicable diseases (NCDs), many of which are chronic, can be prevented or at least delayed – which significantly improves quality of life. The five most common (and usually chronic) NCDs are cancer, diabetes, cardiovascular disease, and chronic respiratory or musculoskeletal disease. These diseases are the primary cause of premature death and chronic complaints.
Counteracting the increase in NCDs – initiating a paradigm shift in healthcare
These five NCDs are the greatest burden of disease on society as a whole. Together with mental illness, they are responsible for 51 % of total health expenditure in Switzerland. This problem is not exclusive to Switzerland. The trend towards urbanisation, the increase in average age and the number of elderly people, as well as changes in dietary and behavioural habits, can be found in many countries. To counter NCDs, we need a paradigm shift in health care, as well as permanent incorporation of prevention into healthcare and rehabilitation throughout the medical care chain. This will make it possible to show chronically ill patients how to cope better with their complaints and alleviate their suffering. People in risk groups will be able to take advantage of a wider range of options for disease prevention. Patients need to be more involved in the treatment process and to agree on goals with the doctor – this is usually more effective than just prescribing medical procedures. The patient's participation strengthens his resolve to take responsibility for his health. The use of interprofessional teams, consisting of doctors and other medical professionals, enables a more holistic view of the patient's (overall) health and can result in a productive enhancement of the doctor- patient relationship. It is also important to reach vulnerable populations, since the incidence of chronic disease is higher than average in such patients, who often have difficulty (for various reasons) in accessing healthcare.
What does "prevention in healthcare" mean?
Increased incorporation of prevention into health care means that both prevention and health promotion (i.e. informing people on increasing their health literacy and encouraging them to take responsibility for their health at home and at work) as well as healthcare are regarded as parts of one system. Or in other words: in future, the current system of acute care and healing should be part of a single system, in which health and quality of life are central values ("from cure to care"). Practices involving prevention and health promotion should become a normal part of primary medical care.
Measures on all levels
This will be achieved with several measures. They involve basic, continuing and advanced training for the medical professions, and also activities, responsibilities and role sharing as well as collaboration between health professionals and their institutions (for example by establishing interprofessional health teams or developing media that enhance communication, such as the electronic patient record/eHealth). However, these measures also involve the participation of patients and their relatives in the respective processes – such as by encouraging self-management and improving health literacy with education or digital aids – and of course the level of funding and monitoring. However, incorporating prevention into healthcare should not result in costly expansion of the programme, but rather in curbing of healthcare costs over the middle and long term. This is because inclusive and well-coordinated collaboration increases the efficiency of primary care. It should be noted that nowadays, not all preventive services that target people with elevated risks or poor health are financed sustainably in the healthcare system. With stakeholders such as the public sector, insurance companies or employers, it is important to develop new funding models that include non-medical consultation and coordination functions.
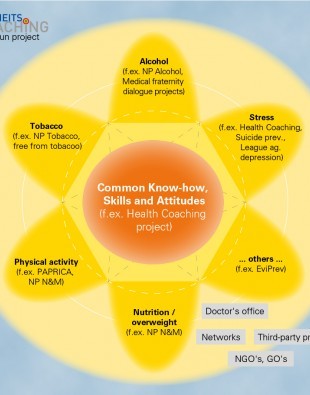
Putting people first
The Health2020 strategy, which sets the priorities of the Federal Council's health policy for the next few years, focuses on the patient: "Healthcare will need to change: with further development of the healthcare system, more thought must be given to the patient's needs". As part of this concept, the NCD strategy aims at a healthcare system that takes into account the changing needs of the patient during his lifespan. To achieve the greatest possible impact, the NCD strategy will be coordinated with addiction prevention (National Addiction Strategy 2017- 2024) as well as prevention of mental illness. The causes of addiction problems and mental illness often overlap with the causes of chronic non-communicable diseases. Approaches that are already used for people with addiction/s or mental illness could be used more often to benefit NCD risk groups.
Improvement without increasing healthcare costs
Implementation of the NCD strategy does not involve re-inventing the whole approach to prevention. However, tried and tested projects should increasingly incorporate additional risk factors if possible, including not only risk factors for NCDs but also those related to addiction and mental health. Innovative projects and programmes that demonstrate how prevention can be better integrated into healthcare need to be supported, improved and promoted more strongly (nationwide if possible) in the context of the NCD strategy. In order that healthcare providers participate in prevention covered by mandatory health insurance, financial incentives for health insurers could be created as an alternative to the existing fee-for-service model. In fact, payers and healthcare providers are being encouraged to develop innovative financing models in this area. Prevention projects are currently supported by Health Promotion Switzerland, the Swiss Tobacco Prevention Fund and the Alkoholzehntel ['Alcohol 10 %' – a Swiss cantonal alcohol prevention fund].
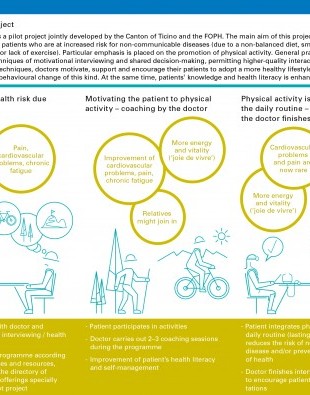
How to integrate prevention into healthcare
How can prevention and healthcare promotion be properly integrated into the healthcare system? The Federal Office of Public Health is developing model healthcare pathways together with stakeholders from the healthcare system, service providers, educational institutions and other expert committees. At the right moment, patients are linked with the relevant professionals by means of these defined pathways. These models are derived from the chronic care model (CCM) and/ or the expanded chronic care model. The model used in the care of chronically ill patients is designed to incorporate several areas in the treatment – effectively and in accordance with the patient's needs. The expanded chronic care model goes one step further, and combines prevention and health promotion more consistently with healthcare. In this case, interprofessional teams (i.e. not just clinically oriented individuals) support chronically ill people with their problems, including those that affect their everyday lives. They may clarify issues relating to healthcare, social isolation or mobility. This approach is intended to significantly improve patient health in the long term. Such continual support also makes it easier to detect signs of dementia or mental health problems. It also means that patients automatically play an active role in their treatment, which in turn improves their self-management and their ability to take responsibility for themselves.
Promotion of interprofessionality and self-management
The increased integration of prevention in healthcare places different requirements on the training and continuing education of healthcare personnel. It is increasingly important to teach and learn interprofessional collaboration in teams – in other words, how several professional groups can work as a team. The Federal Office of Public Health is holding discussions with the providers of educational programmes in various areas of healthcare, in order to jointly define the content and core competencies required for the various occupational groups. With their involvement and participation in appropriate educational activities, patients will be able to develop a different approach to their health. For example, the Swiss Evivo Network addresses chronically ill people and their families with its course "Live a healthy and active life". For its part, the Federal Office of Public Health is planning a coordination platform for entities with an interest in self-management.
Using eHealth, mHealth, and outcome data
The electronic patient record is a key eHealth instrument that simplifies communication between primary healthcare providers – and thus facilitates the interactions of all stakeholders. If doctors, hospitals and pharmacies make patient documents available in a shared system, they can be accessed more easily in case of a subsequent treatment and any findings can be incorporated into the treatment plan. It should be mentioned that rights to the data and access to the patient's electronic health record are at the discretion of the patient. Other eHealth platforms on the issues of prevention and electronic patient files are planned (e.g. EviPrev, a programme for the promotion of evidence-based prevention and health promotion in the doctor's practice, which currently exists only on paper). mHealth tools such as health apps or digital input devices are very useful in the treatment and monitoring of chronic disease. For example, they facilitate rapid intervention in emergency situations, such as when a rapid deterioration of insulin values is observed and reported. The data collected by eHealth and mHealth tools can be used to create health profiles that allow risks to be detected and reduced more rapidly. Furthermore, data on outcomes derived from programmes and projects provide insights into the population that provide a basis for further development of existing and new approaches and models.
Building on experience for the future
The experience that has been gained from the integration of preventive measures into healthcare is very promising. It gives people who are suffering from a chronic illness (or are at risk of contracting one) the ability to cope better with their disease or to reduce their risk of falling ill. They can also be involved in the treatment process and can contribute to preventing complications. They will increasingly be supported by interprofessional healthcare teams consisting of doctors and healthcare professionals. The goal is to increase the patient's quality of life and relieve the load on the healthcare system in the medium and long term, and also to make a significant contribution to curbing healthcare costs.
Contact
Alberto Marcacci
Director Prevention in
Health care Section
alberto.marcacci@bag.admin.ch